Hip Surgery at 37 Years Old
My arthritic/dysplastic hip had a good run but now, it’s time to get an upgrade. At 37 years old, I’ve had a total hip replacement at the Ottawa Hospital (General) and this is my story from one week pre-op to the main event and recovery process. It’s updated regularly. Hoping to share my experience for others who find themselves on a similar path.
FOR THE LATEST UPDATES ON MY PROCEDURE AND RECOVERY, SCROLL DOWN.
WEDNESDAY, MAY 3
8:30 I’m killing time while waiting on a Zoom call from Anesthesia… I will 100% be late for my radio show today (which is on CHEZ 106, weekdays 9A to 2P).
This post will be updated, so bookmark and/or check back often for new content! NOTE: This is all my experience, in my words, from my life. I’ve just turned 37 and will be having a total hip replacement (total arthroplasty, microport, anterior approach) next Tuesday at the General.
CONTEXT: I have been living with seropositive rheumatoid arthritis since 1988 and my body is worn out. The pain is something I’ve written about before:
11:13 Phone call with the pre-admissions Nurse was great. The support staff involved in my upcoming have been a pleasure to deal with. Today I learned that drinking 3 mini-cans of Ginger Ale the night before & in the early morning the day of my surgery might help me heal! That would have been an interesting study to be a part of, eh?
It’s been a while since I’ve had a big operation, C-Sections aside. Sounds like many things have changed. Might be having a spinal block for the operation, which is comforting. I find GA and IVs the most anxiety inducing parts of any type of surgery.
19:35 I’m having trouble focusing on normal work related tasks when I’m not in the office/at the station. I’ve been really draggin’ in the productivity department. I had my routine bloodwork done for an apt. with my GP about non-hip related health concerns (my mouth/face rash situation) and just had more done this afternoon for pre-op reasons at the Civic hospital. Looks like my hemoglobin and neutrophils are Low (again) which is no surprise to me. Hopefully it won’t interfere with my operation.
Tomorrow I start Celebrex to help with pain and inflammation. I had to stop my Enbrel. Saturday I start Pregabalin.
I have also been calling my insurance company a lot to determine what rehab items are covered and how to file a proper claim.
Pre-hab apts are Monday after my radio show and have been ongoing for four weeks - I will obviously have to take some time off to heal before diving back in and rebuilding my strength.
My husband and I also had to settle two separate (and large) mortgage deals (which is a stressful privilege) and open the cottage early as I’ll be out of commission for our typical opening weekend (May 24). Our youngest has dance classes every week and our oldest has tests and a school play to prep for. The internet was out for a couple days because the squirrels ate through the lines, so that was an interesting trouble call.
I am tired. Very tired. I am physically tired and mentally drained.
I am committed to ‘showing up’ at work. I’ve been sick my whole life and I don’t like to let people down. I also don’t like to underperform because of my disease; it is not an excuse and I don’t ever want it to be.
Just having a very hard time staying focused which turns a five minute task into a 50 minute task, etc
THURSDAY, MAY 4
10:43 Received my second info package via e-mail regarding resources for post op care and rehab. 99% of the materials in this package are specifically for senior citizens. I am 37 and this stuff is mentally tough… Hard to focus on work and hosting a 5 hour radio show but there it is.
FRIDAY, MAY 5
19:46 Got to the station early this morning to accommodate an 8:30 phone apt. with a physiotherapist to go over any questions regarding post op restrictions and rehab. The call was very brief. Since my procedure is the anterior approach, I have only two movement restrictions immediately following surgery.
The six week recovery period is to ensure the bone grows around the metal, cementing it in place. Any overdoing it could result in dislocation (barf).
I will be able to use crutches afterall. I’d been told I needed to use a walker (the two wheel, two leg type). Due to my age and fitness level, crutches are preferred but, I’m learning, it kinda depends on who ya ask.
Tomorrow I start the pregabalin for anxiety and nerve pain. That means tonight is my last night to have a drink to “cheers” my busted hip. It has served me well.
If you are reading this, make sure you take some time to appreciate your body and all that it has done for you. Even if it hasn’t been all sunshine and roses.
MONDAY, MAY 8
10:39 Well this was a very pleasant surprise at work today. Hope you caught some of this on CHEZ 106 - also hope you like the Tragically Hip! :)
(My fellow DJs recorded ‘Get well soon’ audio bits which were peppered throughout my radio show today.)
11:53 So many nice messages of support coming through on the radio station text line. I feel the love today! Thank you Ottawa & beyond. I am constantly checking my Ottawa Hospital - My Chart website for any updates on the procedure and I now know the exact beast that will be my new hip… but does it come in black?
TUESDAY, MAY 9
SURGERY DAY
9:05 Since I’m not on air today, I was able to walk my kids to school and watch my oldest sing O Canada with the school before they start their day. I might not be able to do that for a little while, so that was nice. I also received a call from the hospital on my way back home, asking if I could come in earlier due to a change in todays OR schedule.
I’ll be heading in soon! I hope I have the chance to update this blog in stages. But if it so happens that they see me right away and I can’t have my phone - so be it!
Yesterday afternoon, I was contacted by my surgeons office about three research studies I am a good candidate for. Naturally, I agreed to all three. I can’t stress how important it is to be a Lab Rat, if given the chance. I get to play a part in solving health problems and I think that’s so exciting. I agreed to go into the hospital earlier, as yesterday’s surgery time was 2:10PM… so I’ll be in even earlier per this latest phone call - I hope the research team is aware of the change because I believe this stuff is critically important. I’ve been sick for a long time and it’s my hope that future RA kids don’t have to experience the type of pain that I did and do.
I was able to assemble my crutches and get my ice machine going. I’m excited for today. I know it will be painful but the pain I had been living with (without cortisone) was eroding my quality of life.
I feel very blessed and privileged to be going into todays surgery with so much love and support.
I’m writing this from my elliptical machine because every minute counts! I will keep this page updated as I am able.
17:39 Operation was awesome. Success story, so far. In recovery now and it will be an intense few days. I’ll write more when i feel up to it.
Thx for the love and support.
20:26 On my way home now. Feeling good! Taking drugs as needed though (& following a schedule) to get me over the immense pain hump. I wanna stay on top of it because, sometimes, you can get to a point of no return when it comes to pain.
I have a weird sensation that my operated leg is WAY too long but I hear that’s normal. Man, I’ve been disabled for so long & my hip grew improperly that this new way of living is going to take some getting used to!
Thank you for all your well wishes and messages of support and love. I may or may not write you back, as I’m sure you’ll understand: I’m gonna be on DRUGS and a bit busy with recovery!
WEDNESDAY, MAY 10
DAY 1 POST OP
8:31 Yesterday went even better than I could have hoped. All staff were phenomenal and I’d like to give a special shoutout to my Daycare Nurse, Chantal. From start to finish, everyone was remarkable. Being surrounded by positive people aides in a patient’s overall wellbeing, I strongly believe that.
Where to begin… well, if you’ve been following this blog, you’ll know that I was called in extra early so that did throw off some of my research/lab rat duties. I kept telling everyone: “I’m in three studies! You need to make sure they know where to find me! I’m supposed to meet someone at Module X at 11:30!” etc. Even during my operation, I hollered, “Make sure research gets my bones! I promised them they could have them!”
The IV going in was no sweat, though it was one of the first things I asked to be removed after my procedure. Naturally, I had to keep it for a few hours until I met some criteria (walk and do some stairs).
Anesthesia was the very best. I had no issues with the spinal block and got a little woozy in the OR. Because I was awake during the procedure, I was able to voice my ‘woozy’ concerns and they fixed me right up. I swear to GOD I heard ‘Courage’ by the Tragically Hip playing for a while but I might have just been high as a kite. We will never know… haha.
The entire team were a bunch of beauties. It’s a bit jarring to be hoisted up and locked into this stirrups, reminiscent of ski boots. It’s also mildly jarring to hear the saws, drills and hammers but I felt no pain and I enjoyed shooting the breeze with my team.
The whole thing was estimated to take up to 90 minutes and wound up being closer to 45. Wild, eh? I was up and walking in no time, on crutches of course, and even did a small set of stairs. The good thing about being physically disabled for so long is that my good leg knows exactly what to do to help the bad one. It won’t be bad for long! I’ll get my strength back up soon. Today, though, I’m just letting it rest a bit and focusing on pain management and swelling.
I’ll be convalescing at my folks place for a few days and will do my best to keep you updated. I think it’s important to write about this experience as it’s not terribly common for someone my age (37) to go through a total hip replacement. I want to document my experiences to help others.
Ciao for now!
17:40 Oof - ass is being KICKED tonight. Nurse called me and explained that the second day (or today, which I consider the first) is typically the worst. The inner tissue feeling is coming back. As you might imagine, removing bone and hammering a pike into one’s femur doesn’t feel like sunshine and roses.
My focus right now is to control the swelling with my ice machine. I’ve set up a Google voice command to turn it on and off in 15 minute intervals. Have I told you lately how much I love smart home devices? If there is a disabled person in your world, I highly recommend helping them get set up with smart lights and voice commands.
I have a very mild fever and am definitely feeling the pain but I know it is all worth it. I’ll continue to exercise as I am able and increase intensity as I am able.
THURSDAY, MAY 11
DAY 2 POST OP
Ouch. OUCH. I’m taking it slow in terms of the exercises. Some are easy-breezy and others are like I’m a baby learning how to move again (while people poke me with hot knives). The pain is manageable and just a result of the operation itself. Muscle tissue and nerves are moved and sometimes cut (and stitched back together, of course), which causes a lot of pain when trying to do simple movements. My daycare nurse called me yesterday to ask how I was doing and she told me not to push through the pain with the exercises and to do what felt ok/didn’t cause pain.
I am wondering if this is normal and if other’s go through the feelings I’m feeling, like: Will I ever move normally again? Will my leg length be mismatched? When does the pain stop?
I have to remind myself that it’s only been two days. If you want to google the surgery, it was a Total Hip Arthroplasty, Anterior Approach… I accidentally googled it and WHOA MAMMA! You see that stuff and you think, “Ok, yeah, that’s gonna sting for a bit.”
This pain is normal and these questions will answer themselves in time. Not everyone has the same experience, either. We may have had the same procedure but not the same path to recovery and that is okay.
I did my prehab and was in good shape going into the operation, so I think I’m just struggling with the loss of muscle strength and ability I had built up prior to. I know I will be back and better than ever… again, we’re only at Day 2!
12:50 Feeling better & went for a walk outside. It’s very clear why doctors advise not to return to work/normal activity for 6 to 8 weeks. The joint feels good but I really don’t have any semblance of normal or even below average movement at this time. It’ll be six weeks for the bone to grow account the “ball and socket” pieces, cementing them in their permanent place. Any wrong move could jeopardize their (proper) placement.
I’m keeping the loopy drugs for nighttime but Tylenol, Celebrex and Pregabalin are my BFFs during the day. The Pregabalin makes me pretty drowsy - so I am doing my best to avoid making wacky or impulsive decisions (staying away from online shopping, haha).
Following my walk, I had some lunch and am going to use my ice machine for the next few hours; on 15 minutes, off 15 minutes.
19:06 Exercise 6 is killing me. I can’t easily slide my leg out and back in. It’s kinda freaking me out that I can do some of the more complicated tasks (which they ask you to do immediately post op/in hospital) but I can’t do this easier one which the physiotherapist assigned?
Ugh! Limitations are fine and I can accept that it will take a while because my muscles were stretched and some were cut. I will keep working at if. Tomorrow’s a new day!
FRIDAY, MAY 12
Day 3 post op
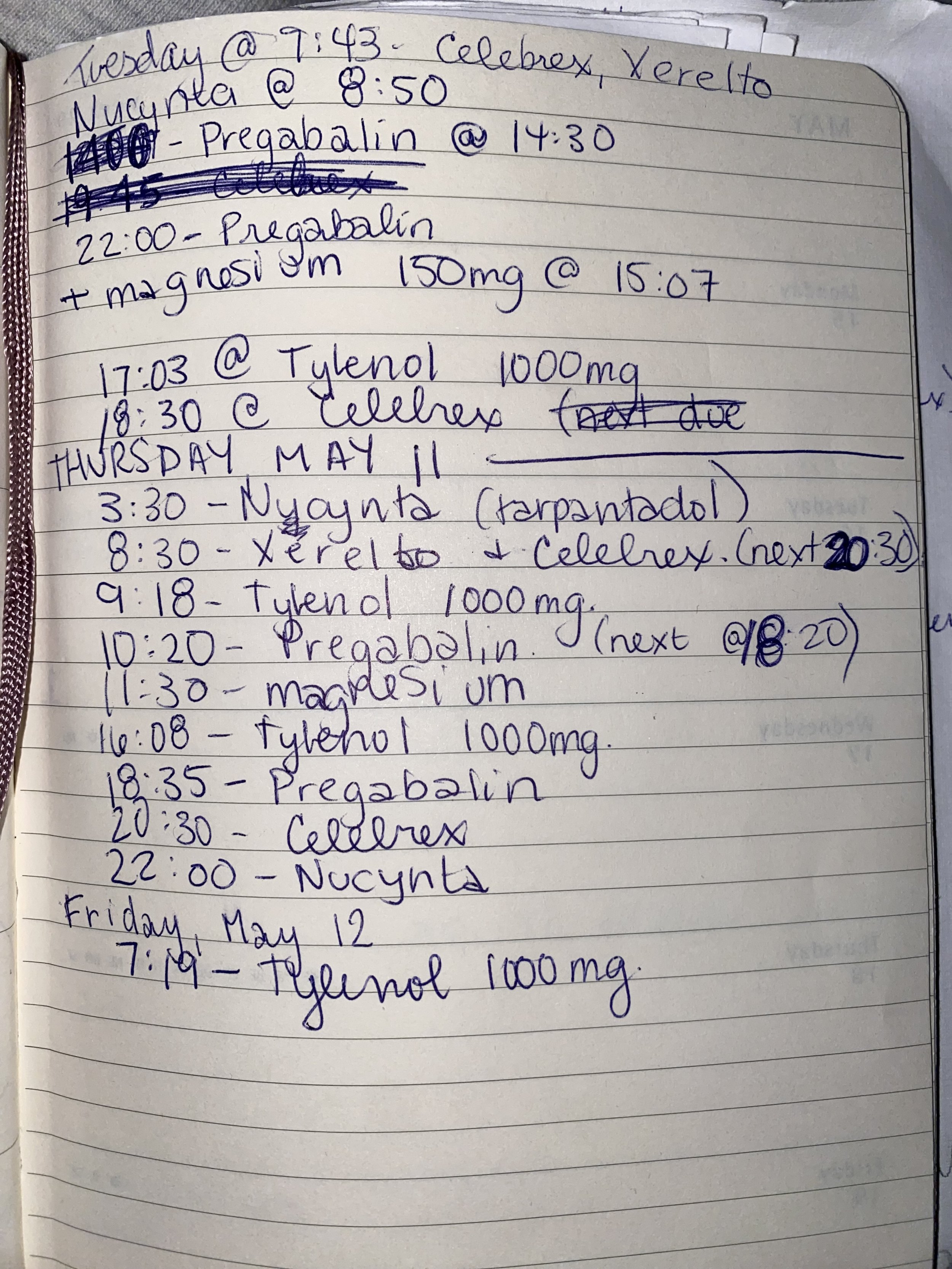
7:39 Had another good sleep but woke up in quite a bit of pain. I’ll try to get that under control without bungling up my medications. My drug schedule looks like this:
Some don’t play nicely together so I have to keep an eye on the clock and make sure everything gets taken in a spaced out manner.
I hope the Tylenol kicks in soon… ouch! I spoke with another new hip recipient about the tricks exercise and they told me that they were not advised to do that one until week two, so I’ve decided to give it a rest until it comes more naturally. I don’t want to do any harm to my new joint.
I have not been able to properly use the bathroom (if you catch my drift) since before my operation. I’m told this is a normal side effect from the opiates and have been taking something to help… it just hasn’t helped yet and my stomach is not happy about it.
All of the pain and inconvenience will be worth it, in the end. There is just no way to get to the end but to go through it. There are not Fast Forward options in life. As I go through this, I’ll do my best to keep you updated on my progress. Hopefully this blog will help others who have total hip replacements learn about recovery and what to expect. I realize that every body is different so I can only speak from my experience.
18:22 Thanks for following these updates. I feel it important to once again say that each body will experience surgery and recovery differently. I have a lot of hope and realize that there is light at the end of the tunnel. I’ve been avoiding taking the heavy duty pain meds but that is a mistake I have made before. I should know better. It has been explained to me by my GP that, due to my disease and drug history, I have a higher tolerance to pain meds. Essentially, I need stronger stuff to scratch the surface of said pain. I always try to go with regular strength stuff - but I’m going to try to remember to take the heavy stuff as needed. That’s what it’s there for. Even if it makes me a little more oogly-woogly than usual, haha.
SATURDAY, MAY 13
Day 4 post op
19:56 Oof. It’s not a walk in the park BUT today reminds me that it’s all going to get better. I need to slow down and TaKe ThE dRuGs.
I spooked myself by taking one of the BIG drugs close to another BIG(ish) drug and lost my vision for a minute (dizzy). So I’ve been really, really spacing them out which is difficult because I am legitimately prescribed a number of post op drugs that I need to take every day (some are wrapping up soon, thank goodness).
I’m walking outside with my crutches but not going very far at all. I am excelling with my exercises (almost pain free). By the time I see Dr. Beaule again (May 26), I should be in much better shape.
Sorry that i didn’t post much today. Ryan (my husband) and our kids came last night and are staying through the weekend. I had planned to go back to the city with them tomorrow but I think I might stay here til mid week. I’m not much help with the kids at this time. Very lucky to have the support I do.
22:16 Sharing WAY too much with this pre-bed update (no, I’m not on the BIG drugs yet, hahah): cannot properly “go to the bathroom” still. I’ve been eating normally and drinking Restoralax every day post op but - yeah… still working on that. It’s a side quest. If you have to take BIG drugs, have a plan for your bowels! Trust me.
SUNDAY, MAY 14
DAY 5 post op
Today I was able to remove my bandage. This scar is pretty intense so I’ll add it to this blog later as a link you have to CLICK ON to see (something I can’t do from my phone). I don’t wanna just embed it here… it’s something you have to WANT to see, haha.
Exercises are getting easier and more pain free. Movement still requires double crutches and will for a while. Operated leg still fees longer but I’m not as worried about that.
My arthritis pain is gone. The surgeon’s job is done! I can focus on healing and get back to enjoying life soon enough.
I’ll keep this page updated with anything noteworthy but, in the immortal words of Bryan Adams, “so far, so good.” (That was the title of his album containing the cancon banger, Summer of ‘69.)
Tuesday, May 16
Day 7 post op
10:09 Everything sucks and I’m dying! Ok - a bit dramatic… I’ve been waking up with very intense headaches for the past three days so yeah, that is the theme of the morning. By this time, I’m feeling much better. I think some things still suck, but I’m getting better matches my 10AM mood… haha.
The first week, post hip surgery has been an uphill battle (with one good leg). My left leg has been a hero and I imagine I look like the Hulk on one side and a skeleton on the right! It’s amazing what our bodies can go through and how they heal. I am very impressed and in awe of what will be a new lease on life with the arthritis pain now gone from my operated area.
But if I’m being honest: the first week sucked. It sucked, big time. If you’re heading into a total hip operation, in my experience - be prepared. Have a care plan. Don’t do exercises that really hurt (even if you’re told to start them right away). Listen to your body because it will tell you what is OK and what isn’t.
I’m walking better. My leg length situation is feeling better. I have less “stabbing nerve pain” when moving/putting weight on my new joint. I can now do all of the exercises (pictured above), mostly with ease.
Everything is getting better but it also is allowed to suck/hurt/be not okay.
In preparation for this surgery, many people told me: “You’ll be pain free!” Feel free to add “but not right after. Right after, it’s going to suck a lot” from me.
Again, this is ALL my opinion based on what I’m living. None of this pain has been permanent. I am in recovery and it’ll be one full week by 1pm today… what my body is doing (while still functioning with autoimmune sickness which will never cease) is truly remarkable.
THURSDAY, MAY 18
Day 9 post op
Feeling the pain in my scar/operated region. Healing happens from the outside in. While I look quite good - there is much healing to be done below the surface and it’s taking a lot from my, energy levels wise.
I have been contributing to work on a programming basis (started that on Monday). While I am not hosting my typical five hour solo, daily radio show, I am putting effort into helping create this weekend’s specialty playlists. This could be zapping my energy but I want to contribute what I can. If I can sit around all day watching TV, I can surely do some work?
My morning headaches are still happening. At least they go away by mid morning. I have finished much of my prescribed meds which allows me to take my pain medicine with less time-based restrictions (little victories!).
As promised: CLICK HERE to see my scar! Only click if you’re ready to see it though because once seen, it can’t be UNSEEN.
SATURDAY, MAY 20
Day 11 post op
I’m back in Ottawa & on air tonight (with CHEZ 106). I am still in Phase 1 of recovery mode which includes a lot of pain, swelling, meds & ice machine in 15 minute intervals (that’s what I’m wearing in the picture). I have very basic physio exercises, which are all now do-able and fairly pain free (not the case last week).
My next apt at the Hospital is Friday to see my surgeon for a progress report and have my stitches removed. If I can enter the next phase of recovery, I think I can resume my arthritis medicine (which will really help me feel 100%), get back to physio with my therapist (in person) and drop down to one crutch.
Hip surgery hurts more the younger you have it done. In my case, it was the only option and I will choose THIS recovery pain (& maybe a bit of a longer leg 😂) over the arthritis pain EVERY TIME.
While the recovery is a grind and the days feel long and exhausting (I’m waking up every four hours for meds) - it’s temporary. I will overcome this. I will heal. I almost cannot believe that I WILL be pain free in my hip. It just doesn’t compute in my brain as a reality right now.
Thanks for your positive notes! I hope you have a great long weekend - do something nice for your body. :)
Friday, May 26
Day 17 post op
Just returned from having my staples removed. Wound healed up very well. I have a bit of suspected fluid buildup when I engage in activity towards the lower part of my scar but it goes away when I give it a rest and should go away over time. It’s not leaking and my leg looks great!
The surgeon who saw me today was in on my operation. It was nice to be able to see the Dr’s face as when I’m in the OR I don’t have contacts in or glasses on so everyone is always a blur but I recognized his voice. He told me that my XRays looked good and encouraged me to get back into physio ASAP and that it was safe to reacquaint myself with the elliptical machine. I haven’t worked out since right before my operation so I’m pretty stoked to start that up again.
The reason I am having a rough time physically and with pain management is because three muscles were interfered with (cut, stretched and/or moved). My hip has never formed properly, so I was walking my entire life in an abnormal way. Now I need to adapt and strengthen these muscles and tendons to allow me to learn how to walk with a healthy hip. Also have to be mindful that my left hip has formed in the same abnormal way, it just was not as bad as my right. The writing is on the wall for my left hip, but I won’t pursue surgery until my quality of life suffers (like what happened with ol’ righty over here).
My leg feeling longer than my non-op leg is also very normal and a feeling that will probably go away once I tighten up the muscles. Doc says I can drop the crutches as soon as I am comfortable with walking/balance. I think I’ll return to the radio station (I’ve been back on air since Day 11 post op) once my crutches are no longer necessary. Hopefully it’ll only be another week or so. I’m going to let physio make that call.
In other words: I’m healing well and am rather unremarkable, which (in medicine, I think) is a good thing. My next apt. and next blog update comes at the end of June, four weeks from today. Stay tuned.
An Update on my Troublesome Hip
Today is the six week anniversary of my (cortisone) hip injection. Dr. Jessica Curran at the Carleton Sport Medicine Clinic walked me through the process and was very pleasant, even though I was pretty tense. Dr. Curran went over my X-rays with me and told me what to expect and I told her that I was probably going to exercise my fight or flight response by laughing. Whenever I’m in pain or nervous, I laugh. It’s a good thing to warn your doctor about if you experience this type of response, too, I’ve learned. The needle to numb the area (lidocaine) was a bit of a pinch, then I started to sweat and chose to ignore the ultrasound screen which the doctor used to guide the needle directly into my hip joint (which entered through my thigh). I hate veins. I get nervous with deep, probing needles even though I’ve had a lot of them.
The whole thing was over in a flash and I couldn’t believe it. I was allowed to stay in the room until my wooziness subsided (less than 10 mins.) and when it came time to walk out, I couldn’t believe how my legs felt: no pain. No pain at all and because I wasn’t in any pain, I didn’t have to limp.
The thing about limping, in my case, is that I do it innately to avoid my hip giving out and to accommodate the pain that I have been living with for the last seven or eight years.
I had previously tried to treat this pain with regular chiro/acupuncture appointments during pregnancy. My chiropractor and I were both under the impression that the source of the pain was my SI joint. This pain often flares during pregnancy. Long story short: it was my hip. My SI joint is fine.
Now, the no pain thing in this instance was thanks to the lidocaine, or as I like to call it (because I’m hilarious), “bone cocaine”.
I walked from the clinic to my motorcycle without limping. Well, I probably still walked with a limp but I really focused on my gate and tried to walk in a “normal” fashion, just to see if I could. It was incredible! Of course, an hour later when the numbing agent wore off, I regretted that. I felt pretty awful and went to bed early.
I didn’t sleep a lot that night. I was very worried that maybe the cortisone wouldn’t work. This hip injection is a precursor to my total hip replacement surgery which I am now in the cue for, for sure this time! The surgeon and I filled the paperwork out together on September 7th. Before my surgeon sent me on my way, he said he’d arrange for this hip injection and cautioned: “If the injection relieves your pain, the hip surgery will be a success. If it doesn’t, we need to find the source of the pain.”
All signs pointed to the hip… so why did I feel like garbage once the lidocaine wore off? I couldn’t fall asleep because I was scared that the cortisone wasn’t going to work. It can take a couple days to kick in, but I have been in such intense pain, constantly, without relief, for nearly 10 years (in my right hip. My RA is also terrible but it comes and goes in terms of how debilitating it can be).
More and more, I read stories about disabled people who choose assisted death because they aren’t really living. They are worn out from the pain. While I don’t see that as an option for me at this time, the prospect of not getting relief from this pain or losing my ability to walk and having hope of meaningful medical intervention and recovery slip away really spooked me. I’m only 36 and I’m more able bodied now than I’ve ever been thanks to my medical team and drug therapies. I have a full time job that I enjoy doing, own a house and a cottage with my husband and we’ve got two awesome, healthy children. I can’t give up hope, you know?
Somehow amidst all of those worrisome thoughts, I was able to fall asleep*, and when I woke up, my pain was gone.
The thing about me is that my lived medical experiences have taught me to never be anything more than “cautiously optimistic”. Surely it’s too soon for the cortisone to be working? Now, I’ve had many cortisone shots back in my CHEO days. They used to put me to sleep to do them because they would inject all of my problem joints in one go. I figured my folks might remember if cortisone was always this immediately effective (providing relief within 24 hours) and, sure enough, my mom tells me, “Amy, you were always like that.”
Be optimistic. Be scared. Be willing to go the distance and be ready to accept limitations. When the time comes to embrace relief, in its many forms: be whatever that is, too.
*The pain I experience is so bad that I do not sleep very well at the best of times. Laying down hurts. I’ve been living like this for at least seven years. The pain creates its own form of fatigue due to my body constantly fighting to “keep going”. Then I have the regular fatigue of someone who can’t get any quality sleep.
Ghost Stories for 2022
Spooky season is upon us and while, I’m 99% ready to start decorating the house, I’m 100% in the mood to start collecting your ghost stories for special Halloween programming on the radio.
If you have a story about something that happened to you that you could not explain, something with a ‘paranormal’ vibe to it, I want to hear it!
There are a few ways for you to share your stories:
Your voice tells your story best: I can call you through my laptop & record our conversation (there are a few ways to do this including Skype, Teams, Zoom, etc.) OR you can record yourself telling the story, and don’t worry about messing up, I will be editing all stories (audio only) for air.
Your story in your words: If you would prefer to tell the story in text, that works too. Send me an e-mail and we’ll go from there.
These Businesses Hire Disabled Ontarians:
Looking to curate a list of employers who actively employ/seek out disabled Ontarians to hire. Can you help me?
— Amy Volume (@amyvolume) May 31, 2022
If you are not on Twitter but wish to respond: amy@chez106.com
Check back for updates. This post will (hopefully) have some employment resources for Ontarians living with disabilities who are seeking employment.
Follow @EARN_UWEO - A United Way East Ontario-led initiative bringing employers and service providers together to increase employment opportunities for people with disabilities.
Here is the comprehensive list of employers who hire persons of all abilities.
Comments from Social Media users:
“I work for a college in the Testing Services department which allows me to support students who require accomodations for any number of reasons and it’s the most rewarding job in the world. I am striving to give [them] the respect and opportunity their deserve to grow and reach their goals.” - Carrie, who is physically disabled.
“I’m a client with Performance Plus Rehabilitative Care Inc. who specialize [in helping] individuals with different disabilities find work. They also have a list of employers.” - Guylaine, living with physical and mental disabilities.
“Check out the Happy Popcorn Co. in Cornwall.” - Daniel
From Happy Popcorn’s website:
“…the cornerstone of our popping was grown from one of the deepest kernels of our heart: our son Jack!
Jack is on the Autism spectrum, and as parents, we wanted to plan for his future. Grateful to be able to open a business inspired by Jack’s love for popcorn, we set out to create a place of inclusion – not only for Jack but for others too.”
“My wife is one of a few disabled people who got hired at TD Place to work as an usher for Redblacks games. They are very inclusive.” - Eric
To add to Eric’s comment, I worked at TD Place for the Compass group when I was laid off by a shuttering radio station. I was the pregnant bartender!
My COVID+ Journey (so far)
This is my day to day experience being COVID+ with rheumatoid arthritis (since 1988), a history of neutropenia and a compromised immune system from taking TNF inhibitor Enbrel for 21 years. Evolving from a COVID story to a Public Healthcare one due to barriers prohibiting access to antiviral medicine for eligible persons (me).
I will be updating this blog entry as my situation evolves. This is mostly for the benefit of other immunocompromised or high-risk persons who are feeling anxious about COVID, pre or post infection. This is all based on my experience and every individual is different.
In this video (six minutes, I am so sorry…), I do my best to explain what my disease is and how viruses are a big deal to those living with autoimmune disease and/or receiving immunosuppressive treatment.
NOTE: This video is OLD. I am not taking my RA meds at this time due to infection.
Thank you to all who have reached out to offer help or to share your story. This has evolved from a ‘oh no! i’m high risk and have COVID’ guide to a ‘how to access help when you need it’ guide.
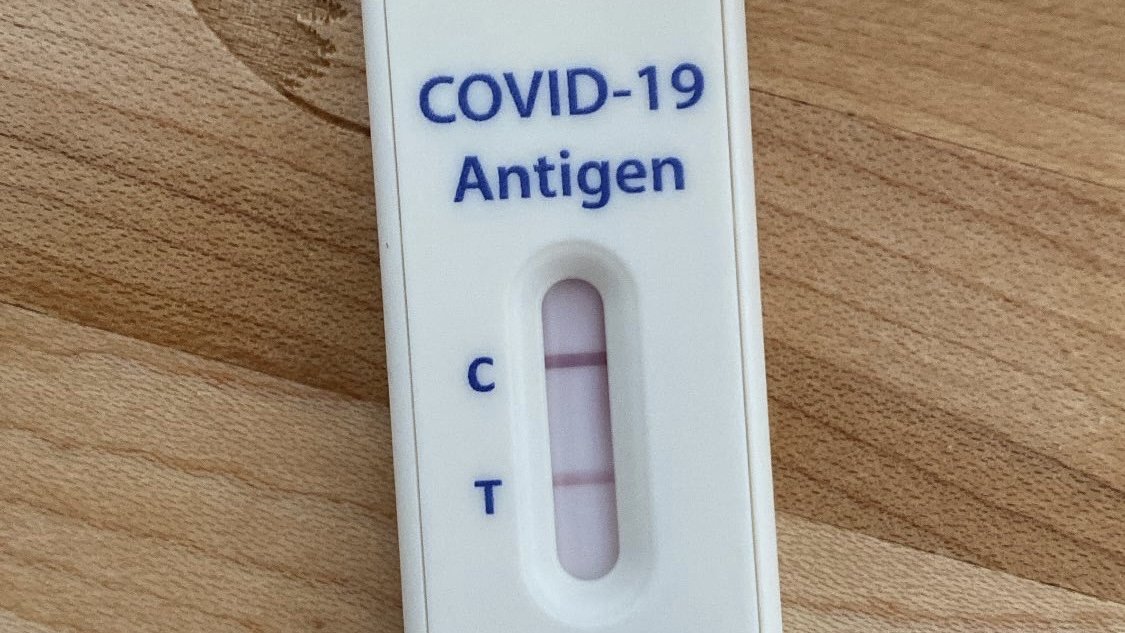
Day 1 - Monday, March 28th: friend who I spent time with on Friday night tests positive for COVID. I take a test which reveals a faint positive but I am feeling okay overall and decide to sleep on it/re-test tomorrow morning.
Symptoms: slight scratchy throat - common with my disease (rheumatoid arthritis) - think nothing of it.
Day 2 - Tuesday, March 29th: I test positive for COVID. I am now convinced.
Symptoms: irritated throat, difficulty sleeping/extreme fatigue, slight sinus congestion (no runny nose), achey (many of these symptoms are part of my daily experience living with RA).
Due to my rheumatoid arthritis or “RA” (autoimmune disease affecting all joints incl. voicebox, organs, soft tissue and blood), ongoing history of neutropenia and twenty one years of immunosupressant therapy of TNF inhibitor ‘Enbrel’, I decide to seek advice from health officials.
8:59AM I have a 20min phone call with Ottawa Public Health Covid Nurse at 613-580-6744 - ontario.ca/exposed
They recommend:
10 day self isolation (ending April 8th, 11:59PM), to keep my daughter (showing symptoms) in iso. with me. Advise that isolation could be recommended for up to 20 days for serevely immunocompromised individuals.
I must be symptom free and feeling better for 48 hours prior to leaving isolation. Two negative RATs must be completed, 24 hours apart, to determine whether or not virus is truly gone.
As long as my husband and our other child do not show symptoms, they are not required to isolate.
Freaking out about the 20 day isolation thing, I decide to call my clinic to try and speak with my GP. No availability until May HOWEVER I somehow score an Urgent Care phone call appointment for 3PM (!!!).
Spoke with Dr. T who understands my situation and completely empathizes with me; prescribes Paxlovid (antiviral treatment) but unsure how to properly procure. It’s a learning curve and not widely available in Canada.
After two callbacks, the amazing Dr. T has secured it for me; says it is issued through Ottawa Hospital Clinical Assessment Centre, handled by outpatient pharmacy (also at Civic), processed and despensed to someone who can receive on my behalf as I, obviously, cannot be out in public. I am told to wait for their call and warned that it can take hours; I say, “No problem!” I am very, very grateful for their efforts and coordination.
Day 3 - Wednesday, March 30th.
Symptoms: Not sleeping well, very scratchy, dry and sore throat (voice impaired), feeling feverish with headache; would compare to a case of strep which I am very familiar with.
Alas, no call from pharmacy last night so I decide to call and check the status of the Paxlovid script. The person I spoke with is kind but tells me they 'do not issue Paxlovid'. They do confirm the existence of the order from doctor but insist I need to receive meds from the clinical assessment centre. It is not possible any other way. In this moment I realize that it was a good idea to make this call!
I call my clinic to leave a message for Dr. T about the prescription issue; they are ALL over it. This is how awesome they are in advocating for me/my treatment:
They are actively trying to push through original order to simply have someone grab medicine for me from hospital pharmacy. (Simplist option).
They are also working to speak with the Director of (1081 Carling) The Ottawa Hospital COVID-19 Therapeutics Centre in an effort to issue the drugs/expedite this process.
They have also submitted a direct referal for me to be seen in person at the COVID-19 Monoclonal Antibody Infusion Clinic.
Concurrantly, my husband books me an apt. at the Moodie Covid-19 Care and Assessment Clinic for 10:30AM. I do not feel comfortable going out in public COVID+ but this feels like the only way to access treatment.
My clinic calls back to say, “Cancel the Moodie apt. They do not issue Paxlovid!” So, I need to be seen at the Ottawa Hospital Clinical Assessment Centre because they do. I explain that I’d tried calling them a few times (yesterday and today) but am informed that I cannot book my own apt. as a patient. It must be done through health clinic/doc office, so they’re trying to get me an apt as soon as possible.
Update: I had to go to bed around 12PM and slept for two hours. I woke with worsening symptoms. Lots of pressure in my sinuses, dizziness and now it is audibly affecting my breathing (no chest pains at this time so no cause for alarm), etc.
The Assessment Centre did not call. My husband decided to follow up 10 minutes before they close and was told to try calling again tomorrow when they open. So that is the current plan.
The breathing ‘noise’ freaked me out as there are pulmonary complications with my disease (co-morbidities which you can learn more about HERE) so I decided to call Public Health to speak with a COVID care nurse. I called at 4:37PM and they stop answering calls at 4:30PM.
It was suggested (by one of you!) that I should try calling Telehealth for some guidance about the breathing thing (which is scary). I was able to speak with a nurse but not in a meaningful way. I actually didn’t get to ask the only question I called for due to the “Answer yes or no to the following” structure of our call which ended with a blunt, “Call your doctor.” The question I was hoping to have answered was: “Considering my disease, neutropenia and immunosuppressive medicine, what should I be on alert for throughout the night as my symptoms now involve my lungs? When should I consider going to the ER?”
6:51PM - I called my clinic back to ask if there were any updates on my file. Was told to call back tomorrow between 1-3PM; confirmed Paxlovid script was faxed to Covid Treatment Centre @ 13:30 - it will be pending and processing until tomorrow
Even mentioning an ER visit tends to rustle jimmies. My system is not healthy and requires intense medical interventions, preferably before irreversible harm is done. I know that I look healthy but I am not. ER visits are not taken lightly by me and the judgement is ill informed.
I’m going to take tylenol, continue to stay hydrated and do my best to sleep through the next few hours before hopefully being seen at the hospital assessment place so I can have antiviral meds to stop this infection before it does permanent damage.
The longer I remain COVID+, the longer I am unable to take my arthritis meds which are the only things keeping me walking/active. I am waiting on two seperate ortho surgeries (foot and hip) which have yet to be scheduled because Ontario’s healthcare system is preserving resources for COVID patients. I can’t access the meds prescribed to me (yesterday) even though I now have COVID.
Make it make sense!!
Day 4 - Thursday, March 31st.
Symptoms: sore, scratchy throat (voice impacted), intense sinus pressure with minor runny nose, itchy lungs, coughing, audible breathing (no chest pain or significant pressure), very dizzy, fatigue.
My son (7 & fully vaxxed) woke us up complaining of chest congestion & issues breathing. He had pneumonia as a baby so I was eager to swab him. His test was negative.
8:05AM - My husband calls the Ottawa Hospital Clinical Assessment Centre to check on the status of my referral. We learn that it is still in triage and are told to call back tomorrow. Tomorrow is Day 5 for me. To be effective, Paxlovid must be started within 5 days of symptom onset.
1:06PM - My clinic calls to check on me (so nice) and to let me know that they, too, called the Assessment Ctr. to check the status of my referral and were told the same (still processing/in triage). So, maybe I will have access to antivirals tomorrow. Maybe I won’t. The clinic did answer my ‘when to go to the ER’ quesiton that I never got to ask Telehealth: if experiencing chest pain or feeling extremely winded.
8:06PM - Just got off the phone with an infectious diseases (yay! rheumatoid arthritis!) physician who is going to help me get this sorted. We had a really nice chat and I am still in awe of how wonderful some people can be. Many have reached out to hear my story and to offer help. I truly appreciate it. I will keep you posted!
In the meanwhile… some light reading from The Ottawa Citizen?
Day 5 - Friday, April 1st.
Symptoms: constant pressure in head/sinus, headache (managed by Tylenol), fatigue (still not sleeping well), chest congestion, dizziness is ramping up, breathing raspy (no chest pain, no cause for alarm), feeling flush (no fever), digestive issues (yes, those ones, neat).
Woke up to an article from CBC featuring my story. Never have I been so acutely aware of my privilidge. As I shared to Twitter,
Lots of you have been trying very hard to help me access antivirals (prescribed Tuesday). Today is my last day for them to be effective. I am cautiously optimistic that I will get them. It happened because I’m privileged to be loud for those in helpful positions to hear. Thank you for hearing my story (so far) & for showing your hearts to those living with disability. Removing barriers is possible when we listen and act together.
8:22AM - I call the Ottawa Hospital Clinical Assessment Centre to check the status of my referral/access to Paxlovid. I am told that my file is still processing. They are going to look into this for me.
9:14AM - I’m contacted from the Assseement Centre and told the order is in for me to receive antiviral drugs and that the pharmacy will courrier the meds to my door. They should arrive by this afternoon. If not, call back (and given direct call-back number).
11:39AM - Received a call from pharmacist with the Civic (they don’t usually call people but wanted to expedite this process in getting me Paxlovid). Very friendly. Very thorough. Again, I am assured antivirals are coming today.
12:30PM - The Paxlovid is here and as of 12:45PM I have had my first dose.
Day 6 - Saturday, April 2nd.
Symptoms: headache, stiffness, sinus pressure draining, congestion lessening, irritated throat, feel warm (no fever), loss of taste and smell.
Day 7 - Sunday, April 3rd.
Symptoms: headache, stiffness (esp. neck), less chest congestion (coughing still but it is “loose”), continued loss of taste and smell, low energy, pain in joints and muscles (but I believe this to be rheumatoid arthritis flaring up).
Day 8 - Monday, April 4th.
Symptoms: fatigue, cough is clearing (very loose), still no taste or smell, body aches (could be the RA).
I sound like myself again, my voice is no longer impacted and my irritated throat is back to normal. My headaches are waning as are most other symptoms. The loss of taste and smell was a late addition to the symptoms list and could have more to do with the Paxlovid? I can’t be sure but WOW, I can taste the pills. I am not complaining! I’ve been on drugs for thirty four+ years, I think I can hack it. I am half way through my antiviral course and since I’ve described everything else in this blog, I might as well describe what I feel while taking them:
Within minutes of taking the pills (two pink, one white) I feel a rush of energy and a ‘drain’ on my sinuses (like someone unplugged the bath). I have not experienced any adverse effects, aside from the intense ‘pill’ taste which has either dominated my pallate (which is why I can’t taste or smell anything else), or perhaps that’s just a late blooming COVID thing. I know it sounds weird to be like, “I can’t taste or smell stuff EXCEPT the drugs!” but that is what I’m experiencing.
I tested myself after lunch today and a very faint positive was the result. I am slowly but surely getting over COVID. Yay!
Day 9 - Tuesday, April 5th.
Symptoms: head clear & chest almost clear of congestion (still coughing up “loose” juice), stiffness remains and I am 99% sure it is my RA, taste and smell still impacted, experiencing more digestive issues (diarrhea… which is maybe a sign the virus is looking for it’s exit?).
Two doses of Paxlovid remain. I will do another RAT tomorrow (Day 9) as the current provincial isolation rules note a 10 Day Isolation (quarantine) for immunocompromised people, which I believe is only 5 for the general public at this time (cause for some confusion).
I will have to test Negative two separate times, 24 hours apart, to be considered fit to leave iso.
Day 10 - Wednesday, April 6th.
Symptoms: low energy, aches, feeling warm (no fever), minor digestive issues, taste and smell still impaired.
Today at 7:42AM I tested negative! Yes! My seven year old, however, has just tested positive. He had pneumonia as a baby so we will be watching him closely as he navigates the next few days. Overall, he is a healthy kid and I expect he’ll do just fine.
CBC featured my story on the National last night.
Day 11 - Thursday, April 7th.
I tested negative yesterday but the symptoms are lingering. For example: my coughing is INTENSE this morning. Worse than it had been the last few days of +. Very itchy lungs; not satisfied with a couple coughs. It’s nasty.
Do I resume my Enbrel now that I’m testing negative? My brain says, “No! Are you kidding? I’m just trying to heal you & you want to gut-punch the immune system with drugs?” but my body is screaming, “Everything hurts! Irreparable damage is happening! **Range of motion is at stake!”
These thoughts create brain clutter which sometimes manifests as anxiety. I work through anxiety with exercise (on good days, when I can move without too much pain), but have been prescribed anti-anx. meds in the past which were very helpful. Anxiety is a co-morbidity of RA.
**Range of motion in terms of rheumatoid arthritis damage refers to the ability to “bend” any joint. This is as far as my wrist will go. Craning beyond this range will break my wrist. You lose joint function with RA & the degeneration of 34 years equals one very sore Amy.
(The text that follows was written when I originally started keeping this diary on Wednesday, March 30th. If you are looking for updates, they will be directly above this text.)
I do not know how long this infection will last. I do not know how severe things will get. I do know that I am COVID+. I am contageous. I don't feel good about going into a hospital knowing this. I also recognize that I am priviliged to have this help and these options.
I am high risk. I have received four vaccines (Pfizer x 3, Moderna x 1). I am cautious but this strain found me. I am lucky that, three days in, I am doing as well as I am (or seem to be; I’m on all the tylenol).
When the pandemic first began (pre-vaccines) I was terrified of getting infected. When you have no natural defence (a functioning immune system), you just don’t stand a chance. I trust in the science and feel very, very lucky to have so many health authorities batting for me. The window to receive Paxlovid treatment is within 5 days of symptomatic infection. I am still only on Day 3 so while I do have time, I am also feeling heightened anxiety about what happens next.
I know that a few of you follow me/my blog because you have an autoimmune disease, are on immunosuppressants or care about/for someone who is high risk. While I didn’t seek out this infection, it did find me so I would like to be open with you during this time in hopes that it helps you with your general anxiety pre-during-post potential infection.
I’m no longer affraid but I am certainly in awe of how many hoops there are for people like me (sick) to jump through during this time.