2024: That’s a wrap
Time to ring in the new year by having more surgery! You may recall me having my hip replaced in May (2023) and how it changed my life for the better… I got into fitness, big time, and have reached new heights in terms of capability, health, you name it. The sky finally became the limit - until I was taken out by a mysterious injury.
Rock radio announcer calls orthopaedic surgeons at The Ottawa Hospital the true rock stars, published October 2023.
It was a few days before we moved out of our Hintonburg house when I experienced a very intense, searing pain in my right ankle accompanied by swelling. I came home from work, sat down to take off my sneakers and BAM - I was out. I had to keep going though; we were moving. We have two kids who were about to be on summer break. I also work full time. ‘Not moving’ is not an option, no matter how much it hurts. This happened June 21st (2024). Some relief came within a few days when I felt (and saw) my tendons ‘pop’ and ‘snap’ near my ankle after forcing it to bend. It was later revealed through examination (by three doctors), ultrasound and MRI technology that I had some bony spurs growing along the back of my right ankle. They have likely been growing for decades but had become so large, they were now forcing my tendons out of place. The relief I felt came only after my tendons began to stretch to accomodate the new bones.
For someone who’s literally never been IN GREAT PHYSICAL SHAPE until this year, I can tell you that it friggin’ sucks falling OUT of shape. I had to change my routine from walking/weight bearing activities to doing a lot on the floor. The cool news is that I now have a pretty strong core - but the crappy news is that I am struggling due to this injury. To anyone reading this who has fallen out of shape; IT SUCKS SO MUCH both mentally and physically.
Per usual, though, there is hope. The light at the end of this tunnel is coming on January 9th; six months post injury, I will be having my bone spurs evicted (debridement) and right toe corrected (fused) at the Ottawa Hospital.
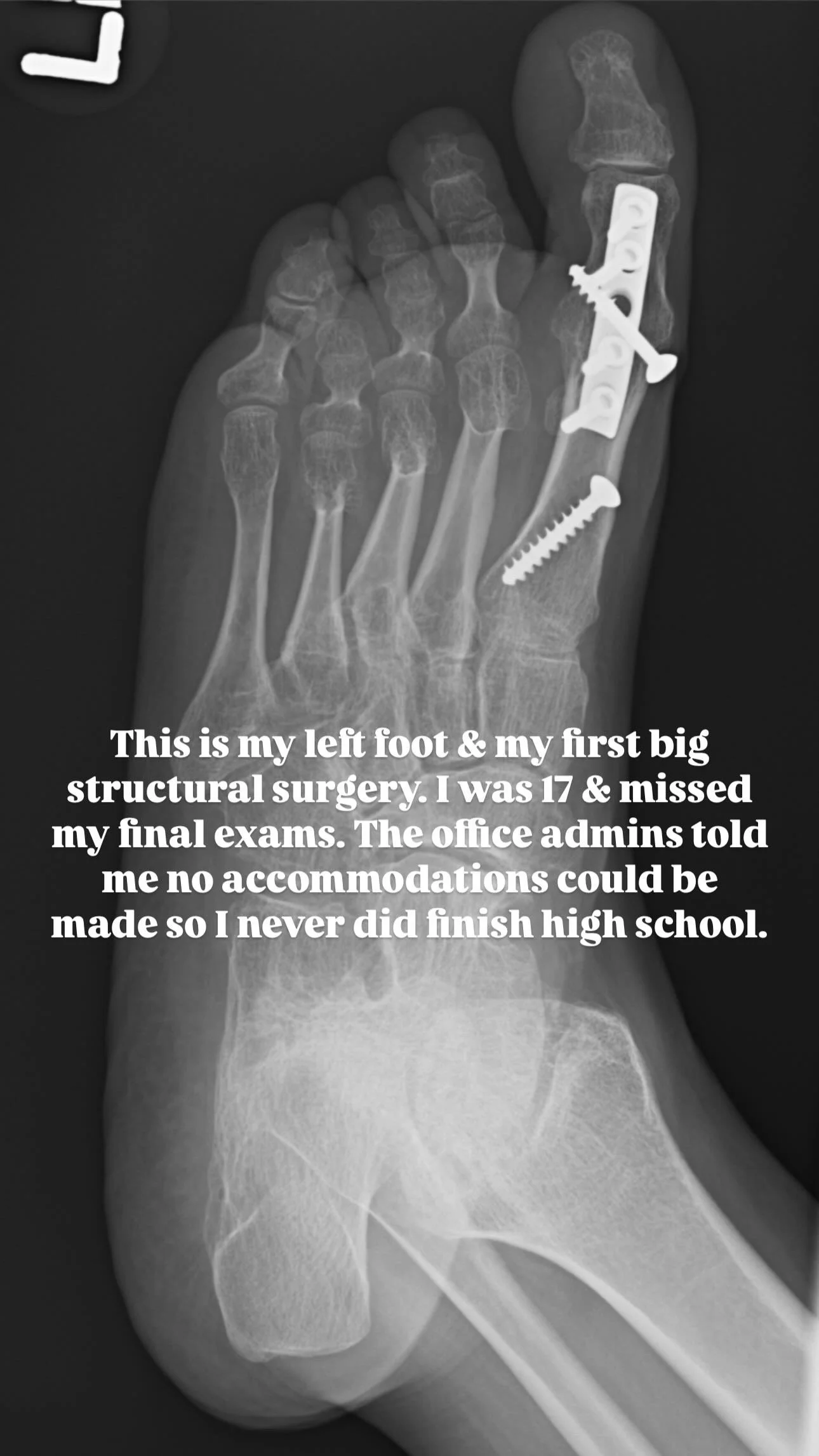
What went from a curious new ailment to ‘we know exactly what that is and how to deal with it” proves that we have world class doctors at home in Ottawa. I have been disabled since 1988 and have, over the years, been very lucky to have assembled a care-team of geniuses with heart. I don’t have surgery because I’m asking for it; I have surgery because my body will not function without it. Surgery is the last resort.
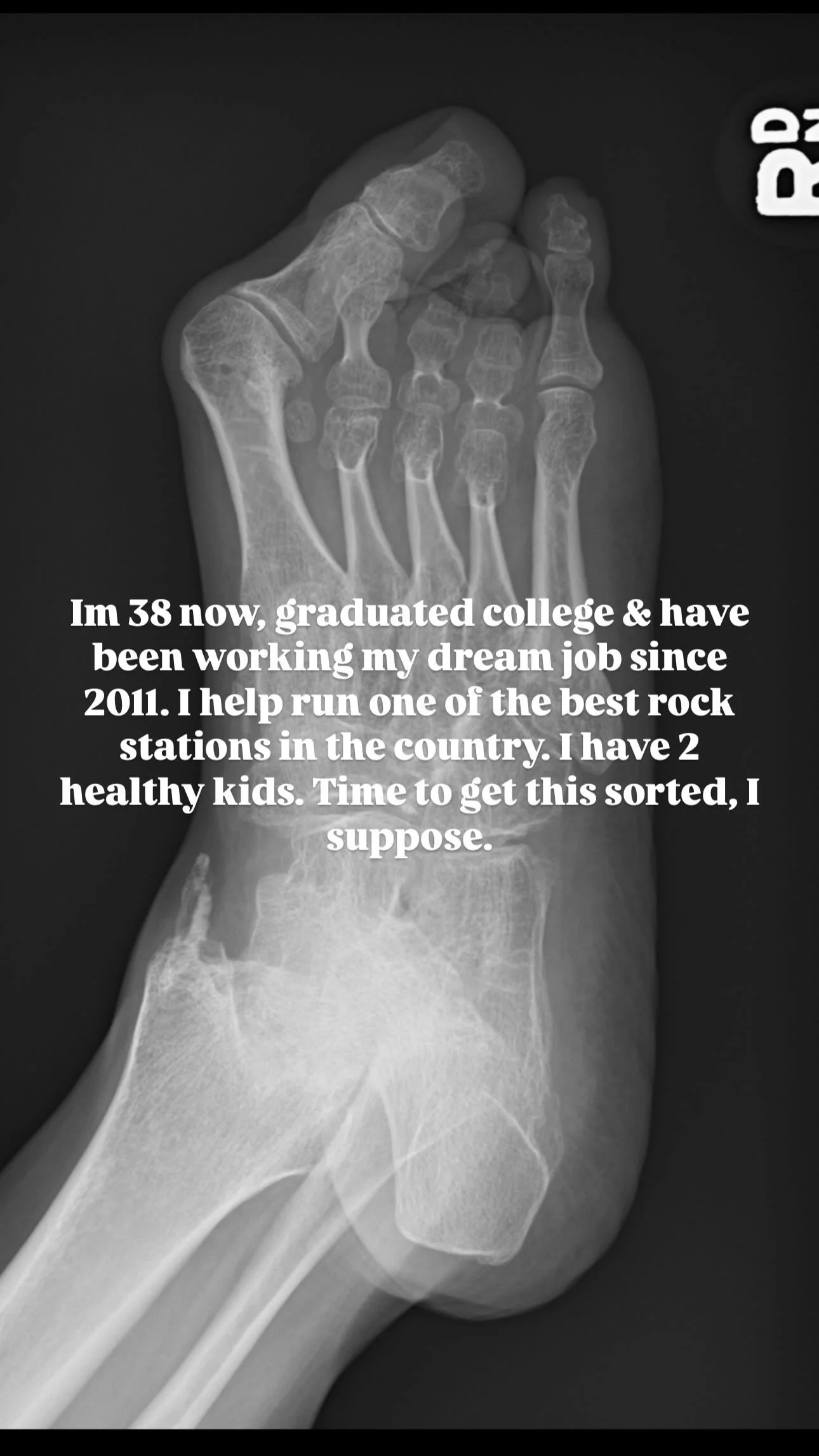
That said… 2025 is going to be brighter. I get to experience getting back into shape. What feels like a mountain to climb ris my focus. Falling out of shape for 6 months has inspired me to get back into it in 6 months, so let’s aim to catch up in June: a year post injury? Watch this blog space for progress reports.
You can also follow along on my instagram account. That’s where I’ll be sharing updates more frequently.
Reminder: I am not a fan of social media and I do not have a Facebook page/profile, nor any presence on Twitter/X. I am not very active on LinkedIn. Instagram remains the only spot where you can follow me: @amyvolume.
Recovery
Oh, hi.
I decided I’d start a new blog for my recovery. If you missed the memo, I had a total hip replacement earlier this month.
So. How am I?
Rough. I’m rough. It’s a painful thing! I know it’s temporary. I know I will be better than OK when I have recovered but I’m still working on it. I’m getting used to a new structure. I’ve never had a healthy joint. How one of my surgeons explained it to me at my 2 week check-up:
“With arthritis, the joint forms as a T. With a healthy hip, the joint is more of a ⊢.” The doctor also went on to explain that the reason my leg feels a bit foreign (and sore) is because three muscles were interfered with during the operation and all of them were stretched to accommodate a proper, healthy joint structure.
Leg length discrepancy is a potential complication with a total hip replacement and I was initially worried about that. Now that I’m three weeks into my recovery, my worries are fading. I know my legs are a similar length and there is no complication there. It is a sensory trick my mind is playing on me because my muscles have been stretched.
It’s a weird feeling, feeling like I’ve been doing yoga or working out all day when I have literally been a slug! Why do my muscles feel like they’ve had a good workout? Because they have. They’ve been pulled. They’re getting used to this new, healthy structure the same way the rest of my body (including my brain) is!
I am very happy with the care I received at the Ottawa Hospital (General). I am grateful for the support I’ve received from my community! I am learning (always learning) that a total hip replacement in a hip like mine with 35 years of arthritis (OA and RA) and dysplasia means a harder recovery; a different path.
Everyone’s body is different and our abilities range. I’m thankful for all that my body has been able to do over the years, in spite of some difficult circumstances. This new hip takes away my extreme pain caused by the disease so what I have to deal with now, in the relatively ‘short term’, is recovering from the procedure. I will adapt to this new structure and I’m so excited to have a healthy joint!
I shared the image (above) recently to show off my scar. This was taken after my 2 week post op check-up where I had my staples removed. This bandage hides a large scar, where the joint went in. I shared it because I want people to see and understand that joint replacement surgeries happen to everyone at all points of life. The overrepresentation of my disease as something that only affects seniors is a huge disservice to all those who are diagnosed at a young age. I was 18 months old, so perhaps I was even born with it? I grew up with the disease AND learning how to navigate peoples ignorance.
Today, I am honoured to share my story with anyone who will listen. There are young people out there wondering what arthritis looks like OR how medical intervention can help OR what to expect with a total joint replacement. I want to be here for you and I hope sharing my experience(s) helps.
An Update on my Troublesome Hip
Today is the six week anniversary of my (cortisone) hip injection. Dr. Jessica Curran at the Carleton Sport Medicine Clinic walked me through the process and was very pleasant, even though I was pretty tense. Dr. Curran went over my X-rays with me and told me what to expect and I told her that I was probably going to exercise my fight or flight response by laughing. Whenever I’m in pain or nervous, I laugh. It’s a good thing to warn your doctor about if you experience this type of response, too, I’ve learned. The needle to numb the area (lidocaine) was a bit of a pinch, then I started to sweat and chose to ignore the ultrasound screen which the doctor used to guide the needle directly into my hip joint (which entered through my thigh). I hate veins. I get nervous with deep, probing needles even though I’ve had a lot of them.
The whole thing was over in a flash and I couldn’t believe it. I was allowed to stay in the room until my wooziness subsided (less than 10 mins.) and when it came time to walk out, I couldn’t believe how my legs felt: no pain. No pain at all and because I wasn’t in any pain, I didn’t have to limp.
The thing about limping, in my case, is that I do it innately to avoid my hip giving out and to accommodate the pain that I have been living with for the last seven or eight years.
I had previously tried to treat this pain with regular chiro/acupuncture appointments during pregnancy. My chiropractor and I were both under the impression that the source of the pain was my SI joint. This pain often flares during pregnancy. Long story short: it was my hip. My SI joint is fine.
Now, the no pain thing in this instance was thanks to the lidocaine, or as I like to call it (because I’m hilarious), “bone cocaine”.
I walked from the clinic to my motorcycle without limping. Well, I probably still walked with a limp but I really focused on my gate and tried to walk in a “normal” fashion, just to see if I could. It was incredible! Of course, an hour later when the numbing agent wore off, I regretted that. I felt pretty awful and went to bed early.
I didn’t sleep a lot that night. I was very worried that maybe the cortisone wouldn’t work. This hip injection is a precursor to my total hip replacement surgery which I am now in the cue for, for sure this time! The surgeon and I filled the paperwork out together on September 7th. Before my surgeon sent me on my way, he said he’d arrange for this hip injection and cautioned: “If the injection relieves your pain, the hip surgery will be a success. If it doesn’t, we need to find the source of the pain.”
All signs pointed to the hip… so why did I feel like garbage once the lidocaine wore off? I couldn’t fall asleep because I was scared that the cortisone wasn’t going to work. It can take a couple days to kick in, but I have been in such intense pain, constantly, without relief, for nearly 10 years (in my right hip. My RA is also terrible but it comes and goes in terms of how debilitating it can be).
More and more, I read stories about disabled people who choose assisted death because they aren’t really living. They are worn out from the pain. While I don’t see that as an option for me at this time, the prospect of not getting relief from this pain or losing my ability to walk and having hope of meaningful medical intervention and recovery slip away really spooked me. I’m only 36 and I’m more able bodied now than I’ve ever been thanks to my medical team and drug therapies. I have a full time job that I enjoy doing, own a house and a cottage with my husband and we’ve got two awesome, healthy children. I can’t give up hope, you know?
Somehow amidst all of those worrisome thoughts, I was able to fall asleep*, and when I woke up, my pain was gone.
The thing about me is that my lived medical experiences have taught me to never be anything more than “cautiously optimistic”. Surely it’s too soon for the cortisone to be working? Now, I’ve had many cortisone shots back in my CHEO days. They used to put me to sleep to do them because they would inject all of my problem joints in one go. I figured my folks might remember if cortisone was always this immediately effective (providing relief within 24 hours) and, sure enough, my mom tells me, “Amy, you were always like that.”
Be optimistic. Be scared. Be willing to go the distance and be ready to accept limitations. When the time comes to embrace relief, in its many forms: be whatever that is, too.
*The pain I experience is so bad that I do not sleep very well at the best of times. Laying down hurts. I’ve been living like this for at least seven years. The pain creates its own form of fatigue due to my body constantly fighting to “keep going”. Then I have the regular fatigue of someone who can’t get any quality sleep.
Hip Surgery Needed
My quality of life is in decline so it’s time to ask for that hip surgery… only the question can’t even be heard right now because our healthcare system is so stressed due to COVID hospitalizations that I am one of thousands of Ontarians being temporarily denied care.
January 15, 2020 I meet with THE hip surgeon. He’s the best in town and does pediatric cases (this simply means cases in people who are young-ish). He tells me that I will require a total hip replacement in my right and we could try a partial in my left but to call in 2 to 10 years (approx.); as soon as my quality of life declines.
Well, almost two years to the day, I called to get in the surgical cue. I know that things are being cancelled or postponed right now due to the pandemic and the strain on our provincial health care system. I simply wanted to get things in order and be on his radar. I am in a great deal of pain and haven’t slept in a long time because laying down causes the pain to spike.
I am doing my best to stay active, which kinda makes the pain worse but I know that if I don’t keep moving, I will lose the ability to move. Period. So I have to kinda continue the cycle of pain - activity - pain - activity - pain because I work, have kids, would like to carry on as normally as possible. Just bought one of those chariot style strollers so that I can stay active. It holds more cargo (and children) than a walker and I’m not needing my wheelchair yet.
This morning I phone the Ortho unit at the hospital and was told to call my surgeon’s office. So I called them and was informed that I need Ortho to ‘assign papers for surgery’ to me. Called Ortho unit back and was put on hold, then told that they don’t really know how to help me at this time and that I should try calling again next week for more information.
The hope in being heard by my care team is all I have keeping me from breaking.
I am trying my best to stay active. I am trying my best to keep smiling. This is not a life saving surgery. I am privileged to have doctors, to not be in a terminal-care-related situation and to be able to work from home.
No one knows when the government is going to actually help out our underappreciated healthcare workers who have been struggling for a long time (before the pandemic, even). These people need to be heard, supported and paid.
This is where we are at in Ontario:
Ontario Temporarily Moving to Modified Step Two of the Roadmap to Reopen - January 03, 2022 - from the Office of the Premier: In addition, on January 5, 2022 the Chief Medical Officer of Health will reinstate Directive 2 for hospitals and regulated health professionals, instructing hospitals to pause all non-emergent and non-urgent surgeries and procedures in order to preserve critical care and human resource capacity.
Ontario tells hospitals to stop non-urgent surgeries, procedures to preserve critical-care capacity - January 05, 2022 - from CBC News, Muriel Draaisma:
In the directive — issued to "regulated health professionals or persons who operate a group practice of regulated health professionals" — Moore says the following steps are required immediately:
"All non-emergent or non-urgent surgeries and procedures should be ceased. Emergent and urgent surgeries should continue, in an effort to reduce and prevent patient morbidity and mortality.
All non-emergent or non-urgent diagnostic imaging and ambulatory clinical activity should be ceased, unless directly related to the provision of emergent or urgent surgeries and procedures or to pain management services."